Abstract
Introduction
Multipotent mesenchymal stromal cells (MSCs) are involved in the formation of niches for hematopoietic stem cells and support hematopoiesis.
There are several reasons for the graft failure in patients after allogeneic hematopoietic stem cell transplantation (allo-HSCT). One of them could be the damage of hematopoietic microenvironment by chemotherapeutic drugs and tumor cells. As a result, the bone marrow (BM) stroma loses its ability to support hematopoiesis.
Perhaps the donor's MSCs can serve as a source of hematopoietic niches recovery in these cases.
The aim of the study was to investigate the possibility to restore the hematopoietic stromal microenvironment in patients with graft failure with donors MSCs implanted into trabecular bone.
Patients and methods
A randomized study for acute graft versus host disease prophylaxis with MSCs has been conducted by the National Research Center for Hematology, Moscow, Russia. MSCs were developed for each patient from their individual BM donor and cryopreserved.
There was long-term BM aplasia observed in 4 patients with GF following allo-HSCT. All of the patients received a second allo-HSCT with MSCs from the donor BM. The MSCs were injected under local anesthesia in the iliac crest that is, directly into the bone marrow in the trabecular bone area. All patients provided informed consent. The implanted MSCs from several passages were thawed and washed free of dimethyl sulfoxide. The cells were then suspended in 2 ml of 6% polyglucin. The cells (200-370 х106) were injected into the bone tissue in small portions (100-200 microliters) through 2 skin and multiple periosteal punctures.
BM punctures were performed for patients 1, 2 and 4.5 months after donor MSC implantation simultaneously. BM (2-3 ml) was collected from 2-4 independent punctures of the iliac spine for each patient. From these BM samples MSCs were isolated and colony forming unit fibroblast (CFU-F) were analyzed according to standard protocols.
The proportion of chimeric DNA was determined in the patients' MSCs at the 1-3rd passages and CFU-F. The cell DNA was isolated by standard methods of extraction and salt precipitation with isopropanol. The chimerism in MSCs was analyzed by the STR-PCR method. The protocol uses reagents for the multiplex analysis of 19 STR-markers and the human amelogenin locus. The informative loci were preselected to monitor the chimerism in the observed patients.
Results
In all 4 cases, after intraosseous injection of MSCs and re-allo-HSCT from the same donor, the patients had a restoration of donor hematopoiesis.
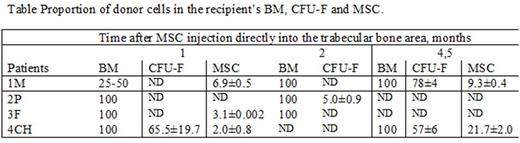
In stromal precursor cells - MSCs and CFU-F, obtained from the BM of patients at 1, 2 and 4.5 months after the implantation of MSCs and second allo-HSCT from the same donor, donors' markers were identified. The table presents the data on chimerism in the BM and studied MSCs and CFU-F in patients.
The sites of BM punctures in patients only approximately coincided with the place of injection of donor MSCs, therefore the proportion of donor cells does not clearly reflect the content of donor stromal cells in patients. Nevertheless, it can be argued that implanted MSCs remain localized at the site of administration and do not lose the ability to proliferate. In fact, these cells survived 3 transfers: from the donor's organism to the culture, then again into the patient's body and repeatedly into the culture. The presence of donor CFU-F - descendants of MSCs proves the functional activity of these cells.
Conclusions
It can be assumed that MSCs caused the restoration of donor hematopoiesis, they probably performed a trophic function, participated in the restoration of niches for hematopoietic cells, or had an immunomodulating effect preventing re-failure of the hematopoietic cell transplant.
Thus, the long-term existence of donor's MSCs in the patient's organism is shown for the first time. A strong potential of MSCs for repeated transfers was revealed. It has been shown that possibly intraosseous MSCs implantation could facilitate transplant engraftment.
The materials are supported by grant from the Russian Science Foundation, Project № 16-15-00102
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal